Cullen S. Hendrix for Denver Dialogues.
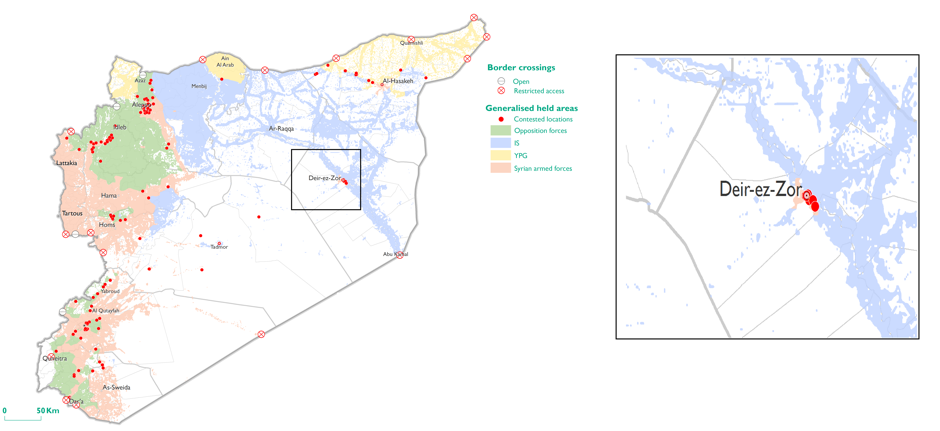
The Democratic Republic of Congo is experiencing what is now the seventh largest Ebola outbreak in history. The World Health Organization is saying the outbreak—located in the heavily conflict-affected province of North Kivu, but spreading to South Kivu and Ituri as well—is occurring in a “perfect storm” of active armed conflict, limiting the ability of relief workers to access exposed populations. As of September 25, WHO staff were only able to reach 20% of individuals in need.
This is not the first time an Ebola outbreak has occurred in a country known for a history of armed conflict. Liberia and Sierra Leone were the epicenter for the deadliest outbreak in recorded history, and the list of Ebola outbreaks reads like a Who’s Who of complex emergencies: DRC, Sudan, and Uganda have all seen large outbreaks since the 1970s. So obviously, there is correlation. But if there is correlation, is that evidence of causation? Does the disease environment in fact cause conflict?
That’s what the parasite‐stress model of intrastate conflict contends. The argument, forwarded by Kenneth Letendre, Corey Fincher, and Randy Thornhill (henceforth LFT), all biologists at the University of New Mexico and published here, here, and here, holds that environments with high disease burdens result in outgroup phobias and encouragement of competition over scarce resources, leading to stronger in-group self-identification (both ethnic and religious) and increased negative perceptions of outsiders. The mechanism is straightforward: in these contexts, “outsiders” are viewed as potential carriers of deadly contagions. This, they argue, is the ultimate explanation for why some countries are more prone to civil war than others. They demonstrate this via empirical analysis of the period 1946-2004, finding that countries with more pathogen stress were systematically more conflict-prone.
The outbreak in the DRC, though tragic, provides a teachable moment regarding two problematic tendencies in social science research: 1) engaging in environmental determinism, and 2) mistaking cause for effect. In this case, the two tendencies converge. I’ll take them in reverse order.
I have no idea whether the parasite-stress (or pathogen severity) model is correct. The logic is intuitively plausible, and it’s an argument that at least has some demonstrable basis in human psychology. But I can tell you that, on the basis of LFT’s analysis, there’s no way to substantiate their claims with respect to civil war. The data on pathogenic severity—their proxy for the disease environment—that underpin their analysis of civil war were collected in 2007. That is, a snapshot taken in the early 21st century that is used to explain conflict in the latter half of the 20th century.
If you’ll pardon a somewhat jocular analogy, this is akin to showing up at the Sigma Chi house on Sunday morning and concluding that red Solo cups and smashed windows cause parties. It mistakes the consequence for the cause.
At least empirically, LFT have the causal arrow reversed: conflict and pathogen severity correlate because conflict has negative effects on the living conditions of persons in conflict zones and diminishes both state and societal capacity to address public health problems. That is, war kills both directly and indirectly, and many of the dead succumb to otherwise preventable or treatable illnesses. This observation is not original to me, and probably not even to the Book of Revelations. And it’s exactly what Kristian Gleditsch and I demonstrated in a response piece in Biological Reviews: using data on malaria prevalence over time, we demonstrated that countries more affected by armed conflict between 1946 and 2004 had made significantly less progress in eradicating malaria over the same period: war prevents gains in public health. By measuring pathogen severity in 1946 and in 2007, we were able to make a more plausible causal argument.
In our view, a more fruitful interpretation of the relationship between disease and conflict is that higher incidence of disease reflects important aspects of poor governance and public goods provision by the state, and that the same shortcomings that lead states to perform poorly in public health also generate grievances and opportunities that make countries more susceptible to violent mobilization.
The more important point—and the one directly relevant for how we interpret conflicts like the several in DRC—relates to the danger of asserting purely environmental causes for social outcomes. The conflicts in DRC may be distally related to the disease environment, and the disease environment may prolong conflicts by sapping government forces’ capabilities, but these conflicts are not “about” disease. They are about legacies of political exclusion, military fractures, the continued fallout of the Second Congo War, and complex patterns of competition over land and mineral resources. That is, they are about the things most civil wars are about: political power and how that power is wielded. Reducing it to disease burden removes human agency from the equation. And given the legacy of treating Africa as a particularly disease-ridden continent, it feeds narratives that are both ugly and unhelpful.
Of course, I’m not arguing that environmental conditions exert no effects on social outcomes like conflict. Indeed, I’d be an odd person to make such an argument. But I am arguing that we should be careful when ascribing environmental causes to political conflict. The current Ebola outbreak in DRC is not a cause of conflict, but conflict is certainly causing it to spread and keeping affected communities from receiving treatment.